While most Americans are shedding their masks and returning to their pre-pandemic lives, Marie Jackson remains in a Chicago hospital room.
She has been there for more than 250 days.
There is no indication yet when Jackson, 53, will be able to go home. She’s waiting on a new pair of lungs; hers were irreversibly scarred when she was sickened by Covid-19 last July.
Full coverage of the Covid-19 pandemic
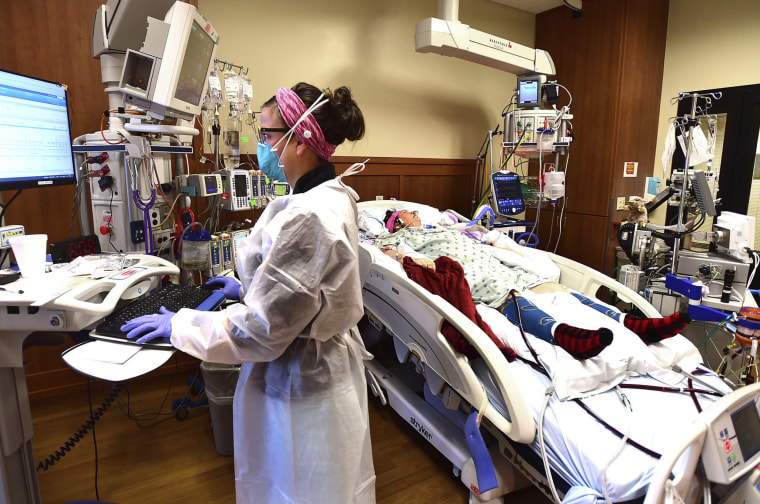
While new Covid hospitalizations are down to their lowest point in the pandemic, Jackson is one of the estimated hundreds of patients who, despite getting sick months ago, remain hospitalized. Their lungs simply cannot heal without mechanical ventilation or other intensive care, such as extracorporeal membrane oxygenation.

ECMO, as it’s called, does the work of the heart and lungs for patients too sick to pump blood and breathe on their own.
Such technology can sustain patients for months, and indeed, many patients have been on ECMO since last summer’s delta wave — at least 10 months in some cases.
But it’s not a permanent solution. ECMO can cause complications, such as infection and blood clots. ICU clinicians work to wean their patients off of ECMO, but sometimes the patient’s body is unable to sustain itself without it. When a patient cannot be weaned from ECMO, new lungs from a donor are necessary.
“You can’t go home on ECMO. You can’t even leave the ICU,” said Dr. Hugh Cassiere, medical director for the cardiothoracic intensive care unit at North Shore University Hospital, part of Northwell Health in New York.
“If you require ECMO for respiratory failure, your only ticket out is through lung transplantation,” he said.
If you require ECMO for respiratory failure, your only ticket out is through lung transplantation.”
Dr. Hugh cassiere
As of February, more than 10 percent of new patients on the lung transplant waiting list wound up there because of Covid, according to data from the United Network for Organ Sharing.
And just over 10 percent of 2,510 lung transplants performed from March 2021 to February have been Covid-related, according to the UNOS data, collected on behalf of NBC News.
Historically, lung transplants have been limited to chronic lung diseases, such as cystic fibrosis, rather than viral infections.
“The need for lung transplantation from patients who have had Covid is really striking,” Dr. David Klassen, chief medical officer for UNOS, said, particularly “for a disease that hasn’t been here very long.”
Covid, it seems, is leading to the need for lung transplantation in two ways. One is a severe complication called acute respiratory distress syndrome, which generally lands people in the ICU early on and can lead to ECMO.
The other is a condition called pulmonary fibrosis. These are often Covid patients who had some degree of lung damage, but who never needed hospitalization.
In these cases, the lung damage persists and progresses over time, sometimes for months. That’s worrisome to Klassen.
“This suggests that there could be a developing need out there that we have yet to appreciate,” Klassen said. “That may increase substantially over time as the millions of people who have Covid continue to recover or not from their illness.”
The vast majority of people currently on the lung transplant waiting list because of Covid are relatively young, between 35 and 64, according to UNOS.
Anecdotally, intensive care physicians still taking care of such patients say their lungs were healthy before their Covid diagnosis.
Hospital strain
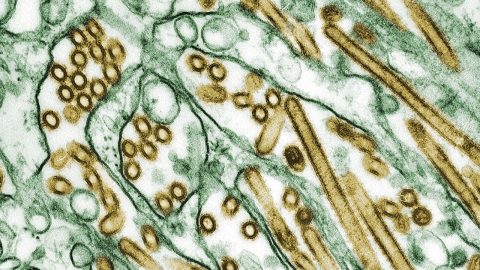
From the beginning of the pandemic, the coronavirus has had a predilection for going deep into the lungs and causing scarring.
Patients hospitalized for Covid for many months can strain hospital resources. In addition to staffing required to monitor the machines 24 hours a day, it takes up to six people, two to three times a day, to get a person on ECMO up, out of bed and moving to at least a nearby chair.
This helps to keep patients’ strength up to a level necessary to be a candidate for lung transplantation. “You have to be able to mobilize to even be considered for a lung transplant,” Cassiere said.
Beyond the strain Covid has put upon the health care system, it’s also upending lung transplant waiting lists.
According to the UNOS data, the number of lung transplants performed each month has remained relatively steady since March of last year. The number of transplants related to Covid, however, has been ticking up.
This suggests that Covid-related transplant candidates are leapfrogging others in need of new lungs.
A person on ECMO goes straight to the top of the list for lung transplant, meaning they could jump ahead of other people who have been waiting longer, such as cystic fibrosis patients, who don’t require the level of intensive care an ECMO patient needs.
Compounding the issue is the shortage of lungs available for transplantation. Lungs are extraordinarily fragile; just 15 percent of the lungs from organ donors are of good enough quality for transplantation, Klassen, of UNOS, said.
Livers, for example, have the ability to regenerate, even after damage. Lung tissue, however, scars easily. Once damaged, it’s incredibly difficult to rebuild fragile lung cells.
‘Unique’ lung damage
Dr. Abbas Shahmohammadi, medical director of the lung transplant thoracic intensive care unit at the University of Florida Health in Gainesville, has had referrals from patients all over the country in need of lung transplants. Just about 40 centers nationwide have done Covid-related lung transplants.
“We see patients with devastating lung injury from Covid that have not recovered despite all supportive care and treatments,” he said. “Eventually, they need a lung transplant.”
Shahmohammadi’s team has performed 33 Covid-related lung transplants.
“What is unique to this virus is the devastating injuries that are prolonged,” he said, adding that he has not seen any other virus cause this level of lung damage.
Physicians at Northwestern Medicine in Chicago, who performed the first double-lung transplant on a Covid patient in the United States, in June 2020, agreed.
By this month, Northwestern had performed lung transplants on 41 Covid patients. The number will likely grow.
“We are continuing to see patients, most of whom have been sick for a while, in the hospital for many months,” Dr. Ankit Bharat, chief of thoracic surgery at Northwestern, said. “They’ve just never gotten better.”
Download the NBC News app for full coverage of the Covid-19 pandemic
Jackson is one of Bharat’s newest prospective lung transplant patients. She was recently transferred from a nearby Chicago hospital.
It was Aug. 1, 2021 — Jackson’s birthday — when her breathing became so labored that a voice inside her told her, “Something is wrong. Freshen up and go to the hospital.”
She’d tested positive for Covid the previous week, during the height of the summer surge of the delta variant. She’d planned on getting vaccinated, but hadn’t done so.
Within days, Jackson couldn’t stop coughing. She struggled to get enough air into her lungs. Listening to that inner voice, she had her son drive her to an emergency room.
“It took every inch of power to walk to the main desk to register,” Jackson said. She was immediately given supplemental oxygen and later was put on ECMO.
On her 259th day in the hospital, Marie Jackson is still undergoing tests to make sure she is a good candidate to get on the waiting list for new lungs.
It is highly unlikely that she will get out of the hospital alive any other way.
“It’s a journey, but I’m a fighter,” Jackson said, her voice weak and raspy. “I have to win. I have to conquer this.”
Follow NBC HEALTH on Twitter & Facebook.







Recent Comments