The hotly anticipated results are in from a landmark pair of major clinical trials of a long-acting, injectable HIV-prevention drug that only requires dosing every six months.
They are sensational.
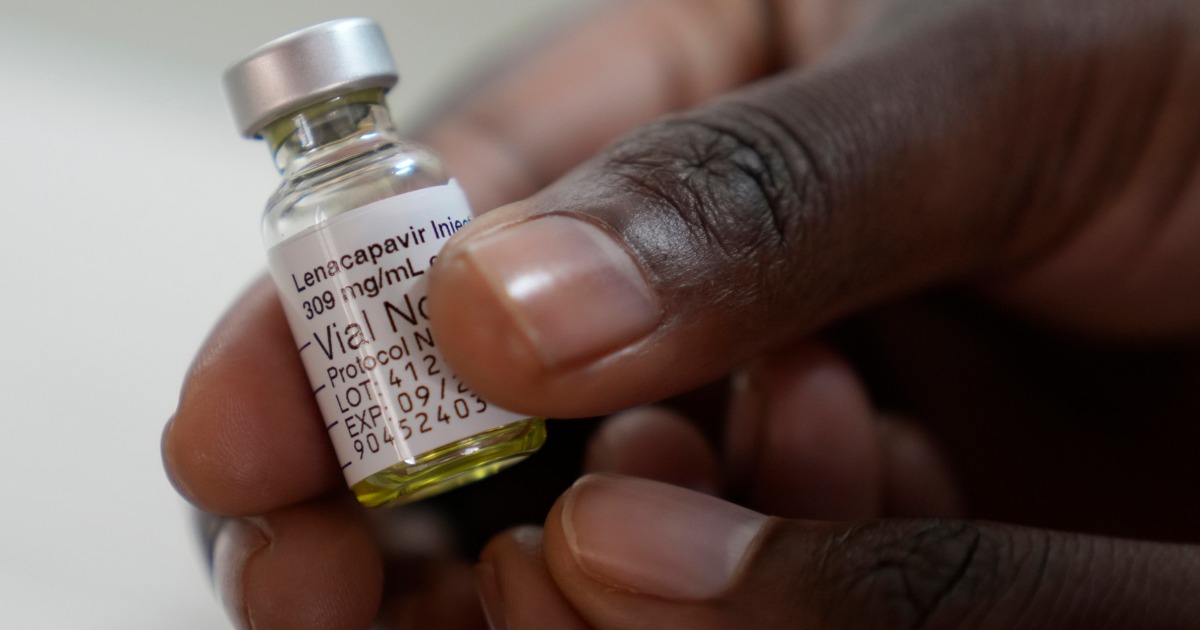
Thrilled over the news Thursday that lenacapavir was 89% more effective at preventing HIV than daily oral preventive medication among gay, bisexual and transgender people, plus previous news that the injectable drug was 100% effective in cisgender women, HIV advocates are looking to the future. They hope that if rolled out broadly and equitably, lenacapavir could be the game changer the nation badly needs.
“These kinds of results are unprecedented,” said Dr. Jared Baeten, senior vice president of virology clinical development at Gilead Sciences, which manufactures lenacapavir. “I have moments like this where I truly am speechless. What this can mean for the trajectory of the HIV epidemic is everything that all the world has imagined for years. We can actually turn off new infections.”
And yet, as battle-worn public health advocates stand on the front lines of an over four-decade effort to finally bring the U.S. HIV epidemic to heel, they find a cold, hard fact staring back at them: Lenacapavir is extraordinarily expensive.
Calling lenacapavir’s clinical trial results “nothing short of amazing,” Jen Kates, director of global health and HIV policy at the nonpartisan health nonprofit KFF, said the news “raises the stakes on the importance of getting this new tool to all those who need it, in the United States and around the world. The track record thus far has unfortunately not been a good one.”
Gilead also manufactures Truvada and Descovy, the two daily oral tablets approved for use as pre-exposure prophylaxis, or PrEP. The pharma giant has already secured approval for the injectable drug in treating highly drug-resistant HIV.
Lenacapavir’s current list price for use as HIV treatment is $3,450 per month. Gilead has not yet indicated whether it will set a different price for the drug’s use as PrEP. A company spokesperson told NBC News on Thursday, however, that the reference point for the price of lenacapavir as PrEP will not be its current use as treatment. It remains unclear whether that statement signals a willingness on the part of the pharmaceutical giant to bring the injectable drug’s price down closer to Earth for its use as HIV prevention.
Given that Truvada has been available as a generic since 2020 and now costs as little as $20 per month (Descovy remains on patent and has a $2,200 sticker price), it remains unclear whether, absent some perhaps novel form of government intervention, insurers will indeed make lenacapavir available widely enough to have what epidemiologists predict could be a sweeping public health impact.
Another injectable drug, ViiV Healthcare’s Apretude, which is dosed every eight weeks, has a $1,965 monthly sticker price and since hitting the market in December 2021 has failed to gain traction in the U.S.
Gilead plans to submit lenacapavir for approval for use as PrEP to the Food and Drug Administration by the end of the year. So this powerful new HIV-prevention tool could hit the U.S. market by mid-to-late 2025.
An HIV-prevention upgrade is badly needed. Since Truvada was approved as the first form of PrEP 12 years ago, the drug has failed to achieve anything in the U.S. approaching its awesome impact on HIV rates among gay and bisexual men in wealthy Western nations such as Australia and the United Kingdom. Those countries boast the type of streamlined sexual-health-care systems that the fragmented U.S. health care system lacks.
“The entire story of PrEP is a missed opportunity,” said Amy Killelea, a health consultant in Arlington, Virginia, and a prominent HIV advocate.
Unprecedented clinical trial results
The advanced clinical trial of lenacapavir in gay men was launched in 2021 at 88 sites across the U.S. and Latin America, and in South Africa and Thailand. It enrolled more than 3,250 cisgender men and transgender and nonbinary people who have sex with male partners.
The participants were randomized to receive either lenacapavir or Truvada on a placebo-controlled, double-blind basis, meaning neither the participants nor the researchers knew who was getting which drug. They were instructed to return every six months for an injection and to take the one dose of the provided pills daily.
A planned interim independent analysis of the trial results indicated that two out of 2,180 participants who received lenacapavir contracted HIV during the trial, as did nine out of 1,087 people who got Truvada. For the lenacapavir group, this represented an 89% lower HIV rate than those in the Truvada group and what Gilead estimated was a 96% lower infection rate than would be expected absent either drug.
Given the clear statistical superiority of lenacapavir over Truvada, the trial’s blinded phase will now be ended several months early. The participants will be informed of which drug they received and provided the option of receiving either going forward.
Lenacapavir proved safe and well-tolerated, with no major safety concerns, according to Gilead. One catch is that the subcutaneous, or under the skin, injection of the drug in the abdominal area leaves a small deposit that can be visible among those with low body fat. It is possible that in real-world use, some will find this off-putting or stigmatizing.
When taken as prescribed, Truvada is over 99% effective at preventing HIV; Descovy is comparably effective. But poor adherence to the daily oral PrEP regimen compromises oral PrEP’s efficacy. And gay and bisexual Black men in particular — the group with the highest HIV rate — have often posted particularly low adherence rates in oral PrEP studies.
The Centers for Disease Control and Prevention estimated in May that between 2018 and 2022, annual U.S. HIV transmissions declined by a modest 12%, from 36,200 to 31,800 cases. Approximately 7 in 10 new HIV cases are in gay and bisexual men, with Black people and Latinos in this group acquiring the virus at much higher rates than their white counterparts. Transgender women, in particular those of color, are also at substantial risk of the virus.
A problem that has bedeviled the CDC and HIV advocates for over a decade is that, in particular given the disproportionately high rates of the virus in their respective demographic groups, Black and Latino gay and bisexual men have never adopted PrEP use at the critical mass needed to truly bring the U.S. epidemic to heel among them. Meanwhile, PrEP has accelerated a long-standing decline in HIV among their white counterparts, exacerbating the gap between the groups.
HIV advocates worry that lenacapavir could only widen such racial disparities further.
“Oral PrEP has been around since 2012. Look at our failure,” said Jirair Ratevosian, an associate research scientist at the Yale School of Nursing. “How do we learn from the past so we don’t squander the opportunity?”
Excitement about lenacapavir’s potential
Dr. Hansel Tookes, a professor in the infectious diseases division at the University of Miami Miller School of Medicine, was the most bullish HIV expert to speak with NBC News about lenacapavir’s prospects.
“I am borderline delusional,” Tookes said of his excitement about how lenacapavir could benefit, in particular, the Southern gay men of color he’s charged with helping protect from HIV.
The South, where the effort to treat and prevent HIV remains hampered by the refusal by seven of 11 states to expand Medicaid under the Affordable Care Act, accounts for half of all new HIV cases, according to the CDC.
“Right now, the challenge is having people take a pill every day to prevent something that they don’t have,” said Tookes of the difficulty of engaging young people in particular in such a banal, forward-thinking routine. “Having to get an injection twice a year is an easier sell.”
Dr. Boghuma Titanji, an infectious disease specialist at Emory University, said she frequently sees new HIV diagnoses in Atlanta, where her university is based, especially among young Black and Latino men who have sex with men.
“These groups often lack access to and information about existing PrEP options,” she said. “While lenacapavir is a valuable addition to our toolkit, for it to reach its full potential, it must be made accessible to those who stand to benefit the most from its effectiveness.”
After Gilead released its initial findings in June from an advanced clinical trial of lenacapavir in cisgender women and adolescent girls in sub-Saharan Africa, HIV advocates immediately put pressure on Gilead to provide the drug at a scalable cost to lower-income nations. This chorus is sure to get louder now that lenacapavir is officially highly effective at protecting gay and bisexual men and trans people as well. Still to come are results from ongoing clinical trials of the drug in people who inject drugs and cisgender women in the U.S.
On Thursday, Gilead stated in a release that the company is committed to delivering “lenacapavir swiftly, sustainably and in sufficient volumes, if approved, to high-incidence, resource-limited countries, which are primarily low- and lower-middle-income countries.” The company is in “active discussions with the HIV community” about these plans.
“It’s not progress if lenacapavir’s cost and other structural challenges impede access, domestically or globally,” said Tim Horn, director of medication access at the public health nonprofit NASTAD. “The results of the drug’s clinical trials, he said, “must be to the benefit of all people at risk for HIV, including those with cost-related hurdles to state-of-the-art prevention and care.”
CORRECTION (Sept. 12, 2024, 3:15 p.m. ET): A previous version of this article misstated the monthly sticker price of ViiV Healthcare’s injectable drug Apretude. It’s $1,965 monthly, not $3,930. The price per injection, which is administered every two months, is $3,930.
For more from NBC Out, sign up for our weekly newsletter.










Recent Comments