
When the Food and Drug Administration recently convened a committee of advisers to assess a cardiac device made by Abbott, the agency didn’t disclose that most of them had received payments from the company or conducted research it had funded — information readily available in a federal database.
One member of the FDA advisory committee was linked to hundreds of payments from Abbott totaling almost $200,000, according to a database maintained by the Department of Health and Human Services. Another was connected to 100 payments totaling about $100,000 and conducted research supported by about $50,000 from Abbott. A third member of the committee worked on research supported by more than $180,000 from the company.
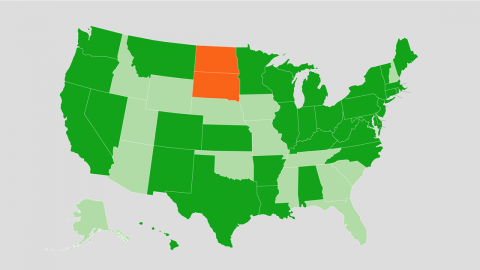
The government database, called “Open Payments,” records financial relationships between doctors and certain other health care providers and the makers of drugs and medical devices. KFF Health News found records of Abbott payments associated with 10 of the 14 voting members of the FDA advisory panel, which was weighing clinical evidence for a heart device called TriClip G4 System. The money, paid from 2016 through 2022 — the most recent year for which the database shows payments — adds up to about $650,000.
The panel voted almost unanimously that the benefits of the device outweigh its risks. Abbott announced on April 2 that the FDA had approved TriClip, which is designed to treat leakage from the heart’s tricuspid valve.
The Abbott payments illustrate the reach of medical industry money and the limits of transparency at the FDA. They also shed light on how the agency weighs relationships between people who serve on its advisory panels and the makers of drugs and medical devices that those committees review as part of the regulatory approval process.
The payments do not reflect wrongdoing on the part of the agency, its outside experts, or the device manufacturer. The database does not show that any of the payments were related directly to the TriClip device.
But some familiar with the process, including people who have served on FDA advisory committees, said the payments should have been disclosed at the Feb. 13 meeting — if not as a regulatory requirement, then in the interest of transparency, because the money might call into question committee members’ objectivity.
“This is a problem,” Dr. Joel Perlmutter, a former FDA advisory committee member and a professor of neurology at Washington University School of Medicine in St. Louis, said by email. “They should or must disclose this due to bias.”
The Open Payments database records several kinds of payments from drug and device makers. One category, called “associated research funding,” supports research in which a physician is named a principal investigator in the database. Another category, called “general payments,” includes consulting fees, travel expenses and meals connected to physicians in the database. The money can flow from manufacturers to third parties, such as hospitals, universities, or other corporate entities, but the database explicitly connects doctors by name to the payments.
At the public meeting to consider the TriClip device, an FDA official announced that committee members had been screened for potential financial conflicts of interest and found in compliance with government requirements.
FDA spokesperson Audra Harrison said by email that the agency doesn’t comment on matters related to individual advisory committee members.
“The FDA followed all appropriate procedures and regulations in vetting these panel members and stands firmly by the integrity of the disclosure and vetting processes in place,” she said. “This includes ensuring advisory committee members do not have, or have the appearance of, a conflict of interest.”
Abbott “has no influence over who is selected to participate in FDA advisory committees,” a spokesperson for the company, Brent Tippen, said in a statement.
Diana Zuckerman, president of the National Center for Health Research, a think tank, said the FDA shouldn’t have allowed recipients of funding from Abbott in recent years to sit in judgment of the Abbott product. The agency takes too narrow a view of what should be disqualifying, she said.
One committee member was Dr. Craig Selzman, chief of the Division of Cardiothoracic Surgery at the University of Utah. The Open Payments database connects to Selzman about $181,000 in associated research funding from Abbott to the University of Utah Hospitals & Clinics.
Asked in an interview if a reasonable person could question the impartiality of committee members based on the Abbott payments, Selzman said: “People from the outside looking in would probably say yes.”
He noted that Abbott’s money went to the university, not to him personally. Participating in industry-funded clinical trials benefits doctors professionally, he said. He added: “There’s probably a better way to provide transparency.”
The FDA has a history of appointing people to advisory committees who had relationships with manufacturers of the products under review. For example, in 2020, the doctor who chaired an FDA advisory committee reviewing Pfizer’s covid-19 vaccine had been a Pfizer consultant.
Appearance Issues
FDA advisory committee candidates, selected to provide expert advice on often complicated drug and device applications, must complete a confidential disclosure report that asks about current and past financial interests as well as “anything that would give an ‘appearance’ of a conflict.”
The FDA has discretion to decide whether someone with an “appearance issue” can serve on a panel, according to a guidance document posted on the agency’s website. Relationships more than a year in the past generally don’t give rise to appearance problems, according to the document, unless they suggest close ties to a company or involvement with the product under review. The main question is whether financial interests would cause a reasonable person to question the member’s impartiality, the document says.
The FDA draws a distinction between appearance issues and financial conflicts of interest. Conflicts of interest occur when someone chosen to serve on an advisory committee has financial interests that “may be impacted” by their work on the committee, an FDA explainer says.
If the FDA finds a conflict of interest but still wants the applicant on a panel, it can issue a public waiver. None of the panelists voting on TriClip received a waiver.
The FDA’s approach to disclosure contrasts with rules for conferences at which doctors earn credit for continuing medical education. For example, for a conference in Boston last month on technology for treatment of heart failure, including TriClip, the group holding the meeting directed speakers to include in their slide presentations disclosures going back 24 months.
Those disclosures — naming companies from which speakers had received consulting fees, grant support, travel expenses, and the like — also appeared on the conference website.
“Unbridled Enthusiasm”
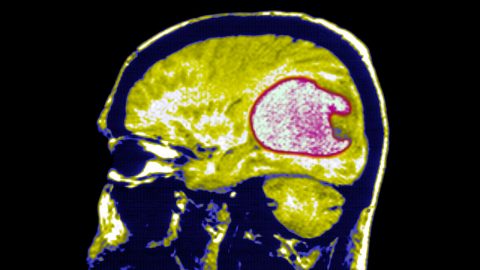
The FDA has designated TriClip a “breakthrough” device with “the potential to provide more effective treatment or diagnosis of a life-threatening or irreversibly debilitating disease” compared with current treatments, an agency official, Megan Naber, told the advisory committee.
Naber said that for breakthrough devices, the “totality of data must still provide a reasonable assurance of safety and effectiveness” but the FDA “may be willing to accept greater uncertainty” about the balance of risks and benefits.
In a briefing paper for the advisory committee, FDA staff pointed out findings from a clinical trial that didn’t reflect well on TriClip. For example, patients treated with TriClip had “numerically higher” mortality and heart failure hospitalization rates during the 12 months after the procedure compared with a control group, according to the report.
Tippen, the Abbott spokesperson, didn’t respond to a request for comment on those findings.
The committee voted 14-0 that TriClip was safe for its intended use. The panel voted 12-2 that the device was effective, and it voted 13-1 that the benefits of TriClip outweighed the risks.
The committee member to whom the database attributes the most money from Abbott, Dr. Paul Hauptman, cast one of the votes against the device on effectiveness and the sole vote against the device on the bottom-line question of its risks versus benefits.
Hauptman said during the meeting that the question of safety was “very, very clear” but added: “I just felt the need to pull back a little bit on unbridled enthusiasm.” Who will benefit from the device, he said, “needs better definition.”
Hauptman, dean of the University of Nevada-Reno School of Medicine, is connected to 268 general payments from Abbott totaling about $197,000 in the Open Payments database. Some payments are listed as going to an entity called Keswick Cardiovascular.
Hauptman said in an email that he followed FDA guidance and added, “My impartiality speaks for itself based on my vote and critical comments.”
Some committee members voted in favor of the device despite concerns.
Dr. Marc Katz, chief of the Division of Cardiothoracic Surgery at the Medical University of South Carolina, is linked to 77 general payments totaling about $53,000 from Abbott and worked on research supported by about $10,000 from the company, according to Open Payments.
“I voted yes for safety, no for effectiveness, but then caved and voted yes for the benefits outweighing the risks,” he said in the meeting.
In an email, he said of his Abbott payments: “All was disclosed and reviewed by the FDA.” He said that he “can be impartial” and that he “openly expressed … concerns about the treatment.”
Dr. Mitchell Krucoff, a professor at Duke University School of Medicine, is connected to 100 general payments totaling about $105,000. Some went to a third party, HPIC Consulting. He also worked on research supported by about $51,000 from Abbott, according to Open Payments.
He said during the meeting that he voted in favor of the device on all three questions and added that doctors have “a lot to learn” once it’s on the market. For instance: By using the device to treat patients now, “do we set people up for catastrophes later?”
In an email, Krucoff said he completed a “very thorough conflict of interest screening by FDA for this panel,” which focused not only on Abbott but also on “any work done/payments received from any other manufacturer with devices in this space.”
Dr. John Hirshfeld Jr., an emeritus professor of medicine at the University of Pennsylvania, is linked by the database to six general payments from Abbott totaling $6,000. Two of the payments linked to him went to a nonprofit, the Cardiovascular Research Foundation, according to the database. He voted yes on all three questions about TriClip but said at the meeting that he “would have liked to have seen more rigorous data to support efficacy.”
In an email, Hirshfeld said he disclosed the payments to the FDA. The agency did not deem him to have a conflict because he had no stake in Abbott’s success and his involvement with the company had ended, he said. Through the conflict-of-interest screening process, he said, he had been excluded from prior advisory panels.







Recent Comments