A few years ago, the organizers of one of the largest U.S. exercise programs for people with Parkinson’s disease realized they had a problem: Most of the students were white.
“We’re always asking who’s not in the room, and why are they not in the room?” said David Leventhal, program director for Dance for PD with the Mark Morris Dance Group in New York City.
Leventhal and his team went to work. They hired more instructors who spoke Spanish or Mandarin and translated marketing materials, which boosted the number of participants from Hispanic and ethnically Chinese communities. But efforts to recruit Black participants haven’t been nearly as effective, Leventhal said.
Exercise is considered fundamental to the treatment of Parkinson’s, with studies showing it can alleviate symptoms of the disease and improve mobility, flexibility, and balance. But people who run Parkinson’s exercise programs in a handful of U.S. cities describe great difficulty in recruiting Black people.
“In Parkinson’s, movement is medicine. So if you’re not figuring out how to engage communities in movement, it’s basically like withholding medication,” Leventhal said. “If this were a pill, there would be an uproar.”

Dance Group / Dance for PD
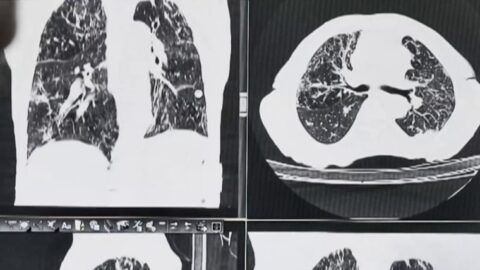
A small study last year by researchers at Yale showed that after six months of exercise, participants’ dopamine-producing neurons — the kind destroyed by Parkinson’s — grew healthier.
This year, research published by a British medical journal encouraged a “paradigm shift” in which exercise would be “individually prescribed as medicine” to patients at an early stage of the disease.
That’s why people like Eric Johnson, founder and CEO of Movement Revolution, are frustrated. Johnson said his Chicago-area initiative offered a free six-month exercise program for Parkinson’s patients and increased marketing in the Black community but got little traction. “It was a challenge,” he said. “I’ll be honest.”
One big hurdle: Many Black people don’t even know they have the disease. The biological and genetic risk factors have long been understudied in people of African ancestry. Recent research identified a novel risk factor for Parkinson’s in the population.
Studies show Black people are less likely to be diagnosed with Parkinson’s. Some point to doctor bias. For example, an article published last year in Nature concluded that bias can influence the evaluation of patients with decreased facial expressivity, a common Parkinson’s symptom in which the facial muscles harden, making it difficult to smile, raise eyebrows, and express feelings.
When a white person shows up at the doctor’s office with such symptoms, a doctor would likely recognize them as signs of Parkinson’s, said Bernard Coley, an advocate for people with Parkinson’s disease, especially those in underengaged communities. But when a Black person has the same symptoms, the doctor might interpret their behaviors as “disconnected” or “angry,” said Coley, who’s on the board of the California chapter of the Parkinson’s Foundation.

Dance Group / Dance for PD
About 1 in 5 Black adults say they’ve been treated unfairly or with disrespect by a health care provider in the past three years because of their race or ethnic background, compared with 3% of white adults, according to a KFF survey last year. The survey also found that 6 in 10 Black adults say they prepare for possible insults and feel they must be careful about their appearance during health care visits, while 1 in 3 white adults say they feel the same way.
Coley said that bias can lead to a delayed or missed Parkinson’s diagnosis, and then once diagnosed, a Black patient might be reluctant to join an exercise program, for fear of retribution on the job.
“You do not want to come off as sick or challenged,” Coley said, “because [your employer] will use any excuse they can to get rid of you.”
Pride and privacy are other factors, said Wendy Lewis, CEO of the Parkinson Council in Philadelphia. “Black and brown families don’t share and tell their business,” she said. “They don’t trust their story with anybody else.”
An important step toward building trust and increasing participation in Parkinson’s exercise programs is for Black people to lead the education and recruitment, said Tammyjo Best, nurse coordinator for the Parkinson’s Disease Comprehensive Care Clinic at Emory University in Atlanta. As a Black person who recruits patients for clinical trials, Best said she often overcomes mistrust.
“When they look at me, they see themselves,” she said.
After his less-than-successful efforts to recruit Black Parkinson’s patients into his exercise program in Chicago, Johnson concluded that the fact that he’s not Black is an “important factor.”
Leventhal, who runs the Parkinson’s exercise program in New York, has come to the same conclusion. His organization, the Mark Morris Dance Group, is fundraising to provide microgrants to groups in underserved communities to start Parkinson’s dance programs, so that “they can become the holder of the purse and the puller of the purse strings and they’re making those financial decisions on their own.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.







Recent Comments