The Centers for Disease Control and Prevention had confirmed 19 cases of monkeypox across 10 U.S. states as of Wednesday.
The country’s first confirmed case was reported in Massachusetts on May 18. The most recent cases were confirmed over the last few days, in Florida, Georgia, Pennsylvania and New York. At least two more cases are suspected, one in California and another in Illinois, but awaiting confirmation via testing.
Although some of the U.S. patients previously traveled to areas where monkeypox has been spreading, that’s not true for every one. Given that, CDC Director Dr. Rochelle Walensky said last week that “we need to presume that there is some community spread.”
“The U.S. has the resources we need to help us respond to monkeypox in this country right now,” Walensky added. “We’ve been preparing for this type of outbreak for decades.”
She highlighted two vaccines that are approved by the Food and Drug Administration for smallpox and stored in the National Strategic Stockpile. The U.S. has 100 million doses of one vaccine, called ACAM2000. The second, called Jynneos, is FDA-approved for use against monkeypox. Some doses of it have already been distributed to close contacts of confirmed cases.
Most of the cases are so far are among men who have sex with men, though Walensky emphasized that “the risk of exposure is not limited to any one particular group.”
“Other communities outside of the LGBTQ community also need to remain vigilant. The transmission can happen whether you are in that community or not in that community,” said Dr. Raj Panjabi, senior director for global health security and biodefense at the White House National Security Council.
What we know about the U.S. monkeypox cases so far
The first U.S. case in the current outbreak was a man hospitalized in Massachusetts on May 12. He remains in good condition, the state’s health department said.
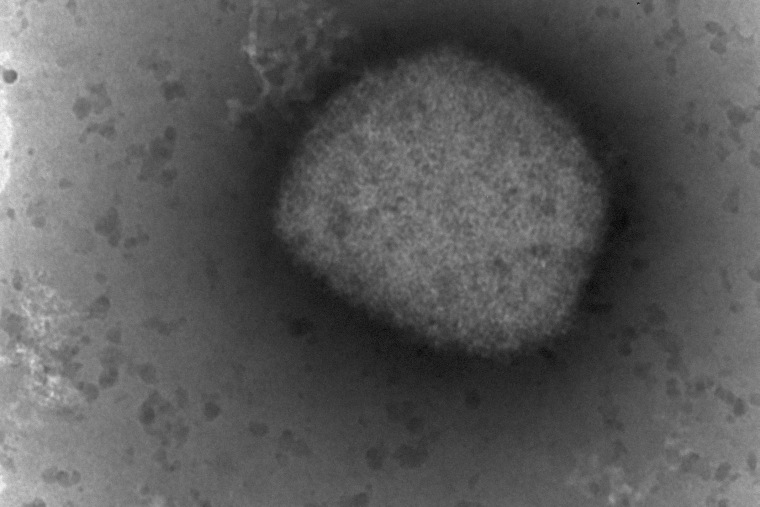
The CDC described his lesions as firm, deep-seated, bumpy and well-defined. In general, monkeypox patients often develop a rash that progresses to small bumps on the skin, followed by blisters that may fill with whitish fluid.
Massachusetts health officials have been investigating more than 200 of that patient’s contacts, most of whom are health care workers.
A senior White House administration official said some doctors at Massachusetts General Hospital were exposed to the man before they knew he had monkeypox, so they weren’t wearing the right protective gear. They were offered vaccines, which could keep them from contracting the disease or developing symptoms if administered shortly after exposure.
Since that case, the CDC has also confirmed four cases in New York, three each in California and Florida, two each in Colorado and Utah, and one each in Georgia, Pennsylvania, Virginia and Washington.
Virginia’s case was a female who had recently traveled to an African country where monkeypox is known to occur, the state health department said.
One of the California patients recently traveled to Europe, and appears to have then spread the virus to two close contacts. Colorado’s first case was a young man who’d recently traveled to Canada, and its second case was a close contact of the first.
Florida’s first case was also related to international travel, the state health department said. The state’s third case was a resident who got tested for monkeypox while in the U.K.
The Utah cases are members of the same household and they recently traveled internationally as well.
Experts are optimistic about containing the outbreak
The CDC said the U.S. patients have all gotten the West African strain of monkeypox, which tends to cause mild disease. Around 1 percent of people who’ve contracted the strain have died in the past, according to the World Health Organization.
The U.S. monkeypox case tally is relatively small compared to some countries in Europe. Spain has confirmed more than 150 cases, and England around 200. In total, more than 770 cases have been confirmed outside of Africa since the start of the outbreak in May, according to Global.health, a group that gathers infectious disease data.
Monkeypox is endemic in 11 African countries, including the Democratic Republic of the Congo, where most of the world’s cases are concentrated. Before this month, the largest monkeypox outbreak in the U.S. was in 2003, when pet prairie dogs infected 47 people.
Infections in Africa typically arise among people who were exposed through bites or scratches from animals, or by preparing meat from wild game. But disease experts think the virus is currently spreading among people via skin-to-skin contact.
People can get monkeypox from exposure to others’ rashes and lesions, which often appear after a patient develops flu-like symptoms. Several recent patients reported rashes in the genital area that did not spread to the rest of the body. That could make the infections less visible, World Health Organization officials said last month.
Experts remain optimistic that the outbreak can be contained through contact tracing and targeted vaccinations.
The FDA approved the Jynneos vaccine in 2019. Though it’s the only one approved for monkeypox, older smallpox vaccines have been shown to protect against monkeypox around 85 percent of the time.
“We’re working hard to contain the cases that are happening so they don’t spread onward,” Jennifer McQuiston, deputy director of the CDC’s High Consequence Pathogens and Pathology division, said last week.
“We continue to watch what is happening and think about whether wider vaccination recommendations would make sense,” McQuiston added. “We have contacts that we’ve identified associated with those cases that would likely most benefit from vaccine, and so that’s where we’re focusing our energies right now.”










Recent Comments