The association technique hasn’t always paid off—but starting in 2007 the gene searches hit pay dirt for sickle-cell. In one study, for instance, a team in Italy studied DNA from thousands of Sardinians (some of whom had beta-thalassemia, another hemoglobin disorder, which is shockingly common on the island) as well from Americans with sickle-cell. When they compared each person’s DNA with the amount of fetal hemoglobin each had, variations kept popping up in one gene: BCL11A.
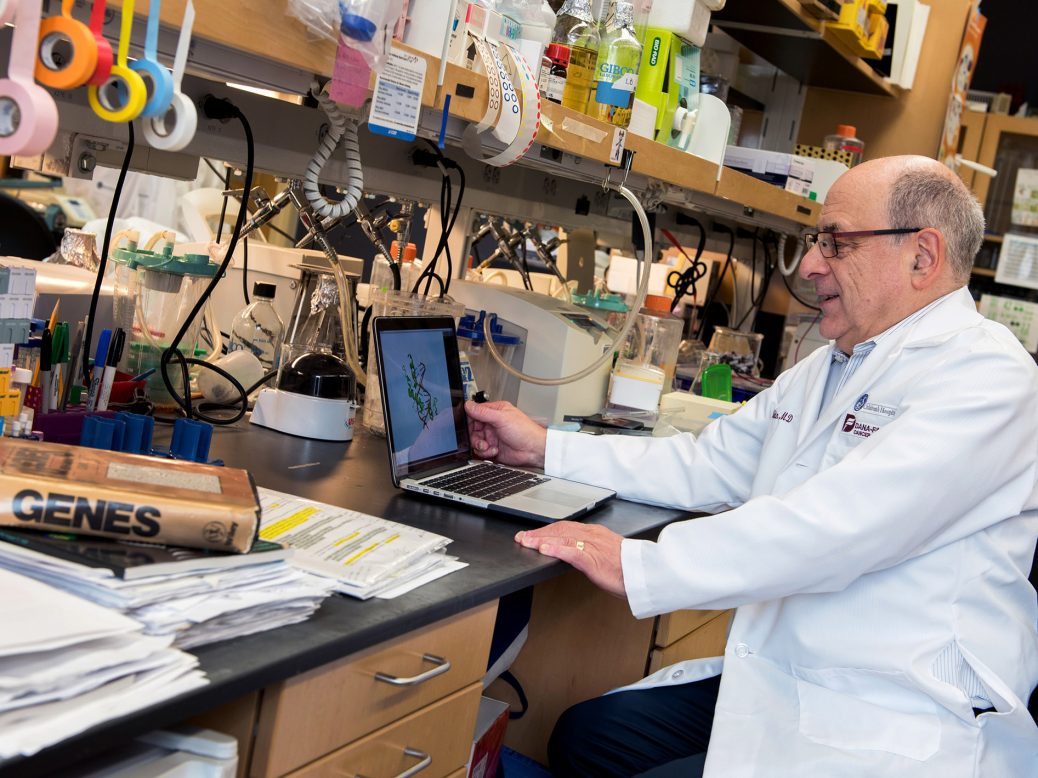
This gene was far from the hemoglobin sequences—in fact, on an entirely different chromosome. And until then, it had been mostly known for its connection to some cancers. It was a complete surprise. “No amount of sequence-gazing would have told you what to look for,” Orkin says now. But the blaring signal told them this could be the control mechanism. Orkin likes to illustrate the impact this clue had with a quote from Marcel Proust: “The only real voyage of discovery consists not in seeking new landscapes but having new eyes.”
All eyes were now on BCL11A. And very quickly, Orkin’s students and trainees showed that it could control fetal hemoglobin. In fact, it was a transcription factor—a type of gene that controls other genes. By shutting off BCL11A they were able to rekindle production of fetal hemoglobin in cells growing in their lab—and later, in 2011, they showed that mice could be cured of sickle-cell in the same fashion. “What this meant is if you could do this to a patient, you could cure them,” says Orkin.
However, in humans it wasn’t going to be as simple as turning the gene off altogether. BCL11A turns out to be an important gene, and losing it wasn’t ultimately good for mice. One study found mice lacking it were mostly dead within six months. But then came another lucky break. Those hits from the Sardinia study? They turned out to cluster in a special region of the BCL11A gene, called an “erythroid enhancer,” that was active only during the production of red blood cells.
Think of it as a gas pedal for BCL11A, but one that is exclusively employed when a stem cell is making red blood cells—a big job, by the way, since your body makes a few billion each day. “It’s absolutely cell specific,” says Orkin. And that meant the gas pedal could be messed with: “We’d gone from the whole genome to one [site] that we could exploit therapeutically.”
Drug target
The switch had mostly been a matter of scientific curiosity. But now researchers at Harvard, and at a company they’d teamed with, Sangamo Biosciences, began to define a treatment. They peppered the enhancer with every possible damaging edit they could—“like a bunch of BBs,” says Bauer, who did the work at Harvard. Eventually, they found the perfect one: a single disruptive edit that would lower BCL11A by about 70%, and consequently allow fetal hemoglobin to increase.
The editing target, a short run of a few DNA letters, never appears elsewhere in most people’s genomes. That’s important, because once programmed, CRISPR will cut the matching target sequence every time it encounters it, whether or not you want it to. Creating unintentional extra edits is considered hazardous, but Bauer says he’s found only one such “off target” site, which he estimates will appear in the genomes of about 10% of African-Americans. But its location isn’t in a gene, so accidental edits there aren’t expected to matter. Bauer thinks the risk, whatever it is, is probably a lot lower than the danger posed by having sickle-cell disease.
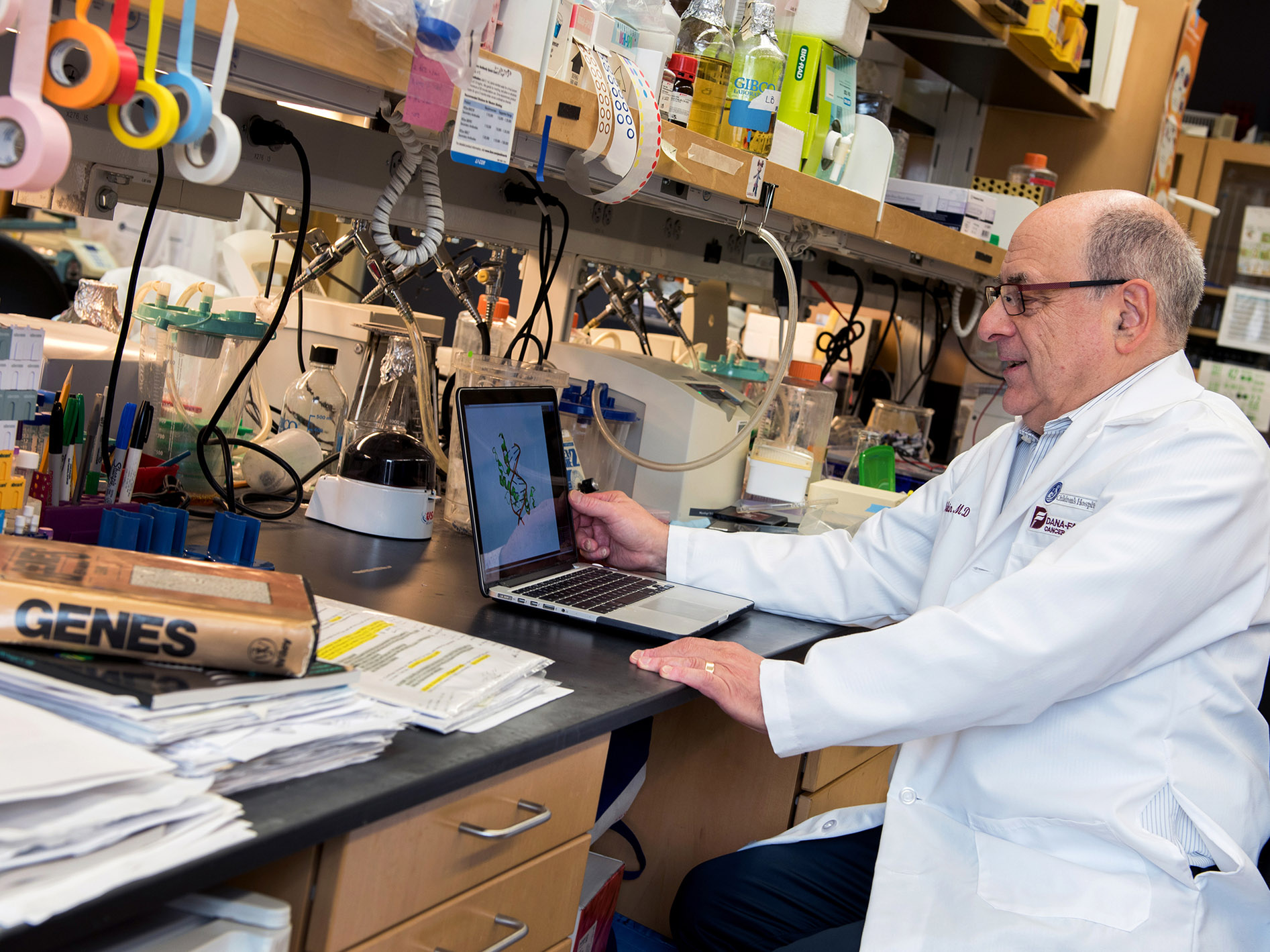
BOSTON CHILDREN’S HOSPITAL
There are signs Orkin’s lab may have found a perfect edit—one that can’t be easily improved on. His institution, Boston Children’s Hospital, patented the discoveries, and later CRISPR Therapeutics and Vertex agreed to pay it for rights to use the edit. They’ll likely contribute royalties, too, once the treatment goes on sale. Orkin told me he thinks the companies tried to develop an alternative—a different, nearby edit—but hadn’t been successful. “They tried to find a better [one] but they couldn’t,” says Orkin. “We have the whole thing.”




Recent Comments